Comments on additional policy and regulatory revisions in response to the COVID-19 public health emergency

Department of Health and Human Services
Attention: CMS 9912 IFC
P.O. Box 8016, Baltimore, MD 21244 8016
To Whom it May Concern:
The HIV+Hepatitis Policy Institute, a national, non-profit organization whose mission is to promote quality and affordable healthcare for people living with or at risk of HIV, hepatitis, and other serious and chronic health conditions, is pleased to submit comments on the interim final rule Additional Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency. Our comments focus on CMS’ interpretation of the law pertaining to the scope of coverage of preventive services (Section 2713 of the Public Health Service) and how it relates to the coverage of Pre-exposure Prophylaxis (PrEP) for the prevention of HIV. HIV+Hep is a member of the HIV Healthcare Access Working Group (HHAWG) and has signed onto its comment letter, which focuses on many other issues contained in the interim final rule.
Support for Implementation of Section 2713 Interpretation
Section 2713 of the Public Health Service Act, which was added by section 1001 of Patient Protection and Affordable Care Act, requires non-grandfathered group health plans to cover without cost-sharing certain preventive services, including those that have a rating of “A”or “B” by the United States Preventive Services Task Force (USPSTF). In the interim final rule, CMS provides additional guidance on the implementation of this provision by stating:
Consistent with the examples provided in the 2015 Final Regulations and sub-regulatory guidance cited in the preamble to the rule making promulgating the 2015 Final Regulations, the Departments further clarify that under the 2015 Final Regulations and this IFC, plans and issuers subject to section 2713 of the PHS Act must cover, without cost sharing, items and services that are integral to the furnishing of the recommended preventive service, regardless of whether the item or service is billed separately. For example, several of the recommended preventive services involve screenings for the presence of certain health conditions, such as diabetes, or a variety of sexually transmitted infections. These recommended screenings, typically performed by laboratories, cannot be conducted without first collecting a specimen. Accordingly, plans and issuers subject to section 2713 of the PHS Act must cover without cost sharing both the specimen collection and the recommended preventive service, regardless of how the specimen collection is billed.
HIV+Hep fully supports this commonsense interpretation and basically clarifies what has been set in practice over the past several years for preventive services, including examples cited in the interim final rule such as the removal of polyps and anesthesia associated with colonoscopies and the laboratory tests needed for cholesterol screening. In each of these examples, CMS clarifies that these ancillary services associated with the actual USPSTF approved service need to be covered without cost-sharing.
Ancillary Services for the Delivery of PrEP
In June 2019, the USPSTF gave a Grade A recommendation for pre-exposure prophylaxis (PrEP), a drug that preventsHIV. All non-grandfathered plans must begin covering PrEP without cost-sharing by January 1, 2021. As described below in this diagram from the CDC, both the FDA and CDC require several additional services associated with the delivery of PrEP to be successful.
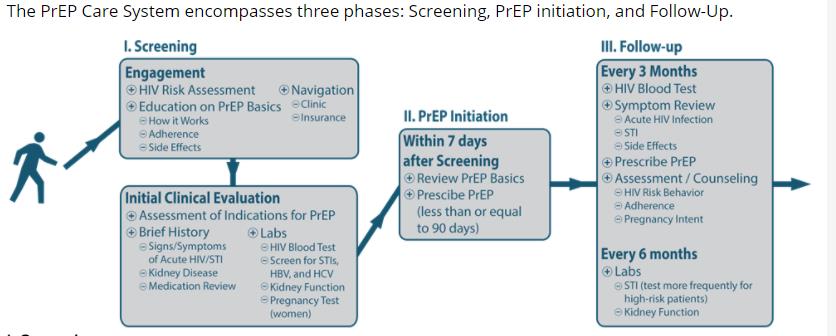
https://www.cdc.gov/hiv/effective-interventions/prevent/prep/index.html#PrEP-Care-System
Therefore, HIV+Hep believes that plans to be compliant with the clarification in this interim final rule must cover these associated services without cost-sharing in the delivery of PrEP. PrEP is not just a drug, but an entire system of care.
HIV+Hep has conducted a cursory review of 2021 qualified health plans and has found that some are not offering PrEP without cost-sharing. Unfortunately, our review of plan formularies could not determine if the insurers were covering PrEP ancillary services without cost-sharing. Some states, including New York and California, have taken steps to inform insurers that they must cover these services without cost-sharing. On the other hand, a regulation in Colorado failed to mention the importance and coverage of these ancillary services. Other states have taken no action. This emphasizes the need for federal clarification, which this interim final rule provides, along with specific guidance regarding PrEP. PrEP is a central component of the Ending the HIV Epidemic Initiative and in efforts to prevent HIV. Everything must be done to ensure people with health insurance who seek PrEP have access to this critical prevention tool, which includes its ancillary services.
The HIV+Hepatitis Policy Institute thanks you for the opportunity to provide these comments. Should you have any questions, please feel free to contact me at cschmid@hivhep.org or (202) 462-3042.
Sincerely,

Carl E Schmid II
Executive Director