Senate testimony on FY25 appropriations for HIV and hepatitis programs

Testimony for the Record
Carl Schmid, Executive Director, HIV+Hepatitis Policy Institute
Senate Appropriations Subcommittee on Labor, HHS, Education, and Related Agencies
Department of Health and Human Services
Fiscal Year 2025 Appropriations for HIV and Hepatitis Programs
On behalf of the HIV+Hepatitis Policy Institute, we respectfully submit this testimony in support of increased funding for domestic HIV and hepatitis programs in the FY 2025 Labor, HHS spending bill.
Our nation can eliminate both HIV and viral hepatitis, but without investing additional resources to accelerate our efforts, we will continue to fall short of these ambitious goals. Increased investment–and certainly not cuts–in surveillance, education, prevention, and care and treatment will lead to further progress in reducing HIV and viral hepatitis, which include taking a syndemic approach to achieve maximum impact.
Thanks to the bipartisan efforts of the Senate in its approach to the FY24 appropriation bills, domestic HIV programs, in the end, were sustained. We urge you to continue that same spirit of cooperation as you proceed with the FY25 bills. We also urge you to proceed in a timely way to prevent uncertainty at the community level which inevitably translates into delays in service and care. While we acknowledge there are spending caps in place, should defense funds be raised, non-defense discretionary spending, which includes HIV programs, must receive corresponding increases as well.
The programs and funding increases detailed below are essential to our nation’s ability to end both these potentially deadly infectious diseases.
Ending the HIV Epidemic in the U.S.
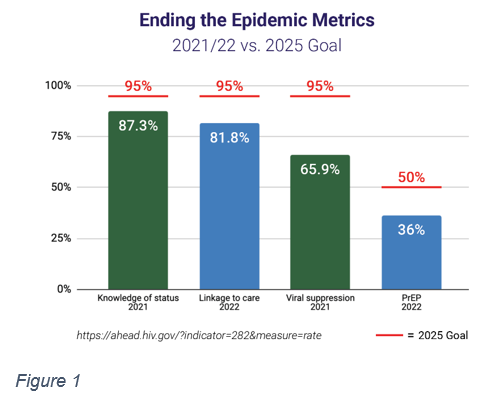
Over the past five years, since it was first proposed by former President Trump and continued under President Biden, Congress has appropriated funding for the Ending the HIV Epidemic in the U.S. initiative, which sets the goal of reducing new HIV infections 90% by 2030. Unfortunately, this funding continues to fall short of what is necessary (Figure 1). The initiative, currently focused on jurisdictions representing about 50% of HIV diagnoses, has shown success with the money appropriated to date. In fact, those phase 1 jurisdictions have seen an impressive drop of 21 percent in new cases since 2017.
The Health Resources and Services Administration’s HIV/AIDS Bureau reports that as a result of this funding, the Ryan White Program brought 22,400 new people into care and re-engaged 15,300 clients. In 2021-2023, the CDC distributed 518,000 free HIV self-test kits and health departments conducted 831,000 HIV tests with 3,000 people receiving a new diagnosis of HIV. The 411 community health centers in 29 states funded through EHE successfully conducted 3.5 million HIV tests, provided PrEP (HIV prevention medication) to 84,800 patients, which represents about one quarter of all people on PrEP in the country, and linked 82 percent of newly diagnosed patients to care within 30 days.
According to the latest surveillance data from the CDC, new HIV diagnoses have fallen by 12 percent over the past five years, driven by a 30 percent decrease in new cases among young people[1]. There was also a 16 percent decrease of new diagnoses in the South since 2018. However, the number of new diagnoses remains high and is not decreasing at the rate needed to end HIV by 2030. Additionally, disparities persist, particularly among gay men of all races and ethnicities, transgender women, Blacks and Latinos. Gay Latino men now account for 39 percent of all HIV diagnoses among men who have sex with men.
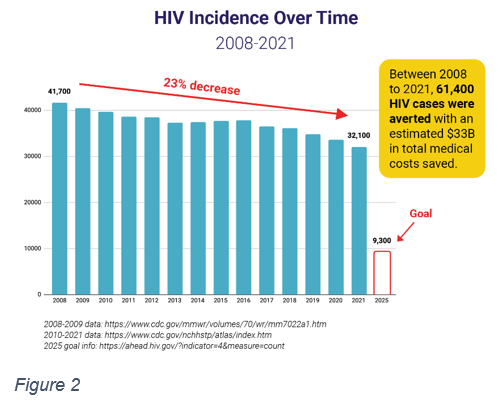
The programs in place with the current funding levels are achieving better health outcomes and downstream savings on the healthcare system (Figure 2). Any reduction in EHE funds will risk serious setbacks in reducing and treating HIV infections, particularly in areas with high concentrations, leading to greater burdens on the healthcare system and even greater demand for federal dollars down the road.
In FY 2024, we urge Congress to fund EHE activities at the levels outlined below to accelerate our efforts to end HIV in the prioritized jurisdictions.
- $395 million for the CDC Division of HIV/AIDS Prevention for testing, linkage to care, and prevention services, including pre-exposure prophylaxis (PrEP) (+$175 million);
- $358.6 million for the HRSA Ryan White HIV/AIDS Program to expand comprehensive care and treatment for people living with HIV (+$193.6 million);
- $207 million for the HRSA Community Health Centers to increase access to prevention services, particularly PrEP (+$50 million); and
- $52 million for the Indian Health Service (IHS) to address the disparate impact of HIV and hepatitis C on American Indian/Alaska Native populations (+$47 million).
PrEP
It is estimated that only 36% of people who could benefit from PrEP have received a prescription. PrEP coverage is highest among White people, while much lower for Blacks and Hispanics/Latinos. PrEP coverage among women is only at 10% of those who could benefit from it. Reducing these disparities must be a priority as we work to expand PrEP use. Increasing CDC’s base HIV prevention and EHE funding, along with HRSA’s EHE funding for community health centers will help ensure PrEP activities can be expanded, particularly for the uninsured. With the average lifetime medical cost for treating HIV over $500,000 per person, PrEP is not only a sound public health measure, but a smart investment of taxpayer dollars.
HIV
The success of the EHE initiative and PrEP delivery rests upon our underlying public health prevention, care, and treatment programs at the CDC, HRSA, and other agencies. Congress must ensure that they are also funded to provide services in all areas of the country.
The Ryan White HIV/AIDS Program at the Health Resources and Services Administration provides medical care, medications, and essential wrap-around services to over 576,000 low-income, uninsured, or underinsured individuals with HIV. Over 59% of clients live at or below 100% of the federal poverty level and nearly three-quarters are from racial and ethnic minority populations. For over 30 years, the Ryan White program has pioneered innovative models of care, which has resulted in over 89% of clients achieving viral suppression. This means someone with HIV cannot pass on the virus, not only protecting others from infection but saving the healthcare system countless dollars. The program is facing increased demand as people live longer and medical inflation continues to rise, but funding has remained stagnant.
This program is especially important in many states, particularly in the South, where there are large healthcare coverage gaps because they have not expanded Medicaid. There are approximately 400,000 people living with HIV who are not engaged in care and treatment. The Ryan White Program can play a large role in bringing this population into care and treatment. Successful HIV treatment ensures that the virus is undetectable, which makes it untransmittable.
We urge Congress to fund the Ryan White HIV/AIDS Program at a total of $3.082 billion in FY25, an increase of $511 million over FY24, of which $194 million is for the EHE initiative and $68 million is for AIDS Drug Assistance Programs.
Increasing funding for high-impact, community-focused HIV prevention services through the CDC’s Division of HIV Prevention remains a priority and results in a strong return on investment. Between 2008 and 2021, there were 23 percent fewer annual new HIV cases, 61,400 cases were averted that saved an estimated $33 billion in medical costs. HIV continues to disproportionately impact Black and Latino gay men, Black heterosexual women, people who inject drugs, and those in the South. There is no single way to prevent HIV, but jurisdictions use a combination of effective evidence-based approaches including testing, linkage to care, condoms, syringe service programs, and PrEP to meet the needs of these populations.
Cuts to these core programs will have deleterious effects in communities and on local health departments including reductions in workforce that include public health nurses and outreach workers who provide much of the on-the-ground surveillance, outreach, and testing that is having such a critical effect on the HIV epidemic. Delays in or lack of services and care will allow infections to rise exponentially and outcomes to worsen among those living with HIV, hepatitis, and related conditions. We urge you to fund the CDC Division of HIV Prevention at $822.7 million in FY25 (+67 m).
A holistic response to the HIV epidemic also depends on fully funding other priority programs at HHS, including the CDC’s Eliminating Opioid-Related Infectious Diseases Program and Division of School and Adolescent Health, the Minority HIV/AIDS Initiative, AIDS Research at the NIH, the Title X Family Planning Program, and the Teen Pregnancy Prevention Program (TPPP).
Viral Hepatitis
We urge you to provide increased funding for viral hepatitis programs at the CDC. The CDC estimates that nearly 5 million people in the United States live with hepatitis B (HBV) or hepatitis C (HCV), and as many as 65% are unaware they are living with the disease. After COVID, viral hepatitis kills more Americans than any other infectious disease and, left untreated, results in significant costs to public programs through liver cancer and liver transplants. Liver transplants were estimated at over $800,000 per procedure in 2021, so, with approximately 1,500 liver transplants annually due to HCV, $1.2 billion avoidable medical costs are being incurred. The opioid epidemic continues to lead to an increase in new viral hepatitis cases. There are several curative treatments available for HCV, but individuals must have access to screening and linkage to care. The president’s budget request includes a proposal for a five-year National Hepatitis C Elimination Program. As Congress considers this program, we must shore up public health funding now for hepatitis.
The viral hepatitis programs at the CDC are severely underfunded, receiving only $43 million—far short of what is needed to build and strengthen our public health response to all forms of hepatitis. Increased investment would allow the CDC and the states to enhance testing and screening programs, conduct additional provider education, enhance clinical services specific to hepatitis at sites serving vulnerable populations, and increase services related to hepatitis outbreaks and injection drug use. We urge you to provide the CDC Division of Viral Hepatitis with $150 million, an increase of $107 million over FY24 enacted levels.
Federal HIV & Hepatitis Coordination
Two important offices which coordinate the implementation of the NHAS, EHE and viral hepatitis activities need resources to bolster their ability to coordinate HIV and viral hepatitis activities across the federal government. We urge you to provide a total of $20 million (+$12 m) for the HHS Office of Infectious Disease and HIV/AIDS Policy and $3 million for the White House Office of National AIDS Policy in FY25.
SAMHSA HIV Block Grant
We urge you to include language that was proposed in the president’s budget that would modernize the way in which states qualify to be eligible for the HIV set-aside of the Substance Use Prevention, Treatment, and Recovery Services Block Grant (SUBG). Instead of using the outdated measurement of AIDS cases for a state to qualify for the 5 percent HIV set-aside, the number of HIV cases should be used. Due to the current language, only three states and the District of Columbia now qualify. With the update, up to twenty would be able to.
In conclusion, we urge the committee to continue its investment in our nation’s public health infrastructure specifically as it relates to addressing the ongoing HIV and hepatitis epidemics.
[1] HIV Surveillance Supplemental Report: Estimated HIV Incidence and Prevalence in the United States, 2018–2022, May 21, 2024